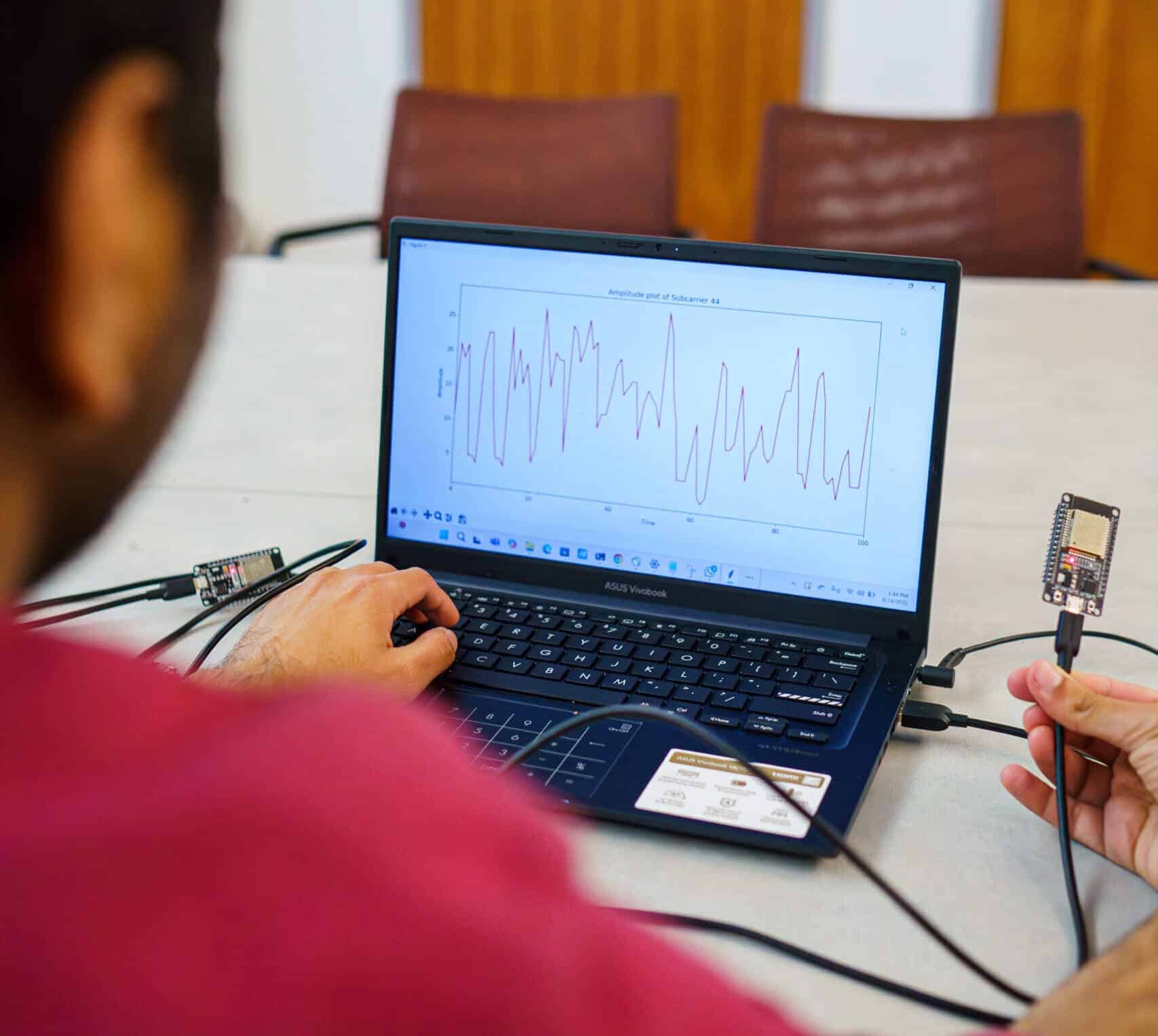
A system called Pulse-Fi captures a person’s heartbeat from up to 10 feet away using only Wi-Fi signals and machine learning algorithms. The prototype operates with very low-cost hardware (ESP32 chips costing $5–$10 or Raspberry Pi around $30) and maintains accuracy across 17 different postures and scenarios.
The idea that a router could “listen” to a heartbeat without any device on the wrist might sound like science fiction. However, a team from the University of California, Santa Cruz (UC Santa Cruz) has developed Pulse-Fi, a system that measures heart rate using Wi-Fi signals with clinical-level accuracy—all without wearables, bands, or contact sensors. Their work was published in the proceedings of the IEEE International Conference on Distributed Computing in Smart Systems and the Internet of Things (DCOSS-IoT) 2025. It points toward a future where monitoring vital signs at home could be non-intrusive, affordable, and ubiquitous.
A “wireless stethoscope” already at home
The technical premise is brilliantly simple: any Wi-Fi device emits radio waves that propagate through the room and are minimally disturbed when passing through objects and people. These perturbations are mathematically detectable at the receiver. Pulse-Fi relies on a Wi-Fi transmitter and receiver that capture subtle variations in the channel caused by small mechanical torso movements and blood volume changes associated with heartbeat. With a filtering pipeline and a machine learning model, the system separates environmental noise from the heart signal.
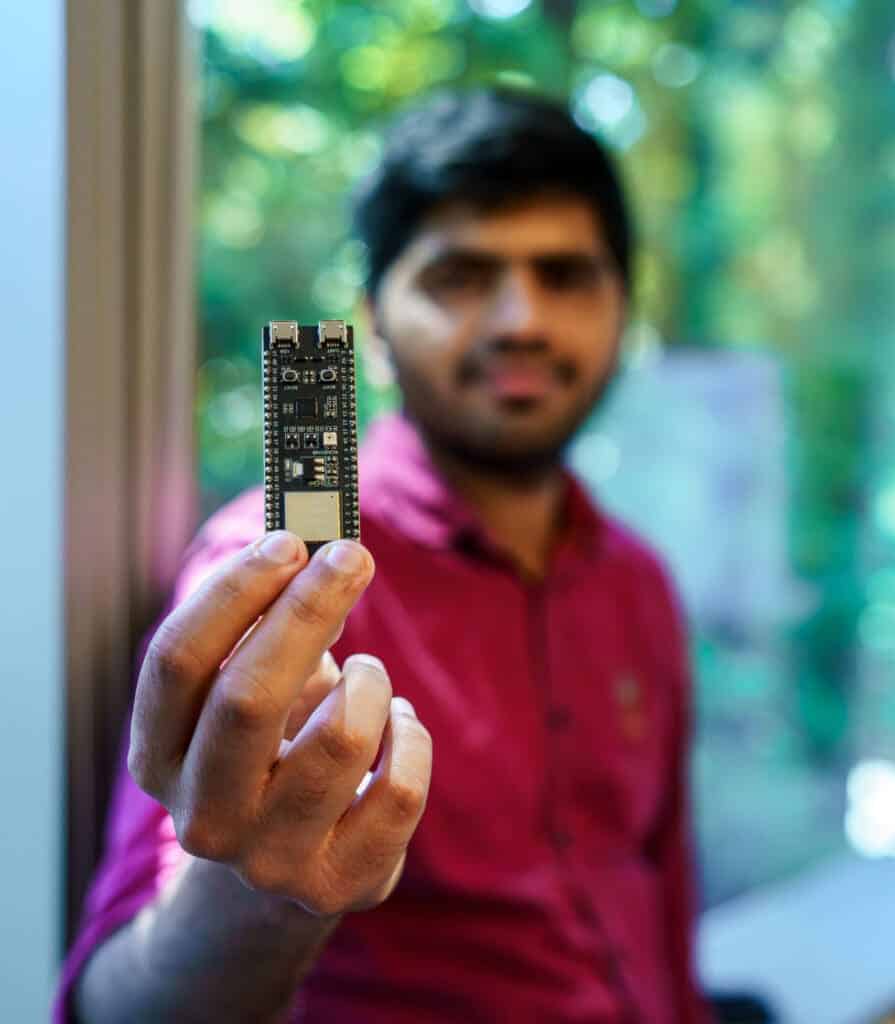
The team—led by professor Katia Obraczka, with doctoral student Nayan Bhatia and pre-university researcher Pranay Kocheta— emphasizes the affordability of their approach: ESP32 boards (Wi-Fi modules costing between $5 and $10) and Raspberry Pi (~$30). In testing, Raspberry Pi offered even better performance, thanks to its radio and processing power. The key achievement is demonstrating that clinical measurement quality does not require expensive equipment.
118 people, 17 postures, 5 seconds to accurate measurement
The study extended beyond the lab. The authors recruited 118 participants and, using an oximeter as ground truth, trained and validated their algorithm across 17 positions and scenarios: sitting, standing, lying down, walking, with the device placed in various room locations up to 10 feet away. The landmark result: after just 5 seconds of signal, the estimated pulse rate has an average error of only 0.5 beats per minute (bpm). The more data collected, the greater the accuracy.
Two features stand out for their robustness:
- Distance (up to 10 feet) does not significantly degrade performance thanks to the machine learning model.
- Posture and context — so variable in daily life — do not disrupt measurements, overcoming challenges faced by previous approaches using radar or Wi-Fi.
This is a quantitative leap for low-resource environments: monitoring heart rate with cheap routers at home, in clinics, or in assisted living settings—where wearable devices and multi-parameter monitors lack budget. And it does so contactless and without user intervention, mitigating a common obstacle to telemonitoring adherence.
From home to clinic: potential use scenarios
Heart rate is vital for physical activity, stress, hydration, fever, or drug reactions. A Wi-Fi system that measures pulse in the background opens specialized applications such as:
- Passive home monitoring: elderly people, patients with heart failure, arrhythmias, or Anxiety could benefit from early alerts without wearing devices.
- Hospital rooms or residences: ubiquitous coverage using existing Wi-Fi infrastructure offers a redundant layer alongside traditional sensors.
- Telemedicine and digital health: households where wearables are rejected, allergic, or forgotten could transmit reliable metrics without changing routines.
- Low-resource settings (refuges, emergencies, middle-income countries): with ESP32 or Raspberry Pi, enable basic screening at minimal cost.
What about privacy? Wi-Fi sensing the environment
Any technology that “observes” without a camera raises ethical questions. Pulse-Fi does not record video or audio: it analyzes derived metrics from wireless channel responses. Still, inferring physiological activity with household devices warrants guarantees such as:
- Consent and local control: processing on the edge (device-side), with no data uploads by default; explicit opt-in.
- Data anonymization/seudonymization when shared with doctors or caregivers.
- Privacy by design: hardware switches, activity LEDs, access logs, and end-to-end encryption during transmission.
The authors invite interested parties to contact UC Santa Cruz’s innovation office to explore commercialization. This suggests a future regulatory pathway—governed by medical standards and data protection laws—if Pulse-Fi becomes a medical device.
Why now? The leap with data and edge ML
Many studies have attempted to “measure with Wi-Fi.” What makes this approach different?
- Own and third-party data: The team created their ESP32 dataset, absent in literature, and validated with an independent dataset from Brazil using Raspberry Pi (the most extensive Wi-Fi pulse dataset, according to authors). This fills a key data gap.
- Better-designed machine learning pipeline: Pulse-Fi filters environmental noise and isolates heartbeat signatures using robust models applicable across distances and postures.
- Edge computing: Raspberry Pi’s local processing allows real-time analysis without relying on cloud infrastructure, crucial for privacy and latency.
Current limitations… and future goals: respiration detection
While achieving an 0.5 bpm error in just 5 seconds is impressive, the team acknowledges that Pulse-Fi is still a prototype. Next steps include:
- Expanded clinical validation with specific populations (elderly, cardiac patients, children).
- Testing under real interference: homes with multiple routers, multiple people, complex walls, and furniture.
- Longitudinal studies: how does the signal change with network alterations or relocations?
In parallel, they are working to extend the technique to detect respiratory rate and apnea events. Preliminary unpublished results are promising. Combining pulse and breathing measurements could enable simple sleep screening at home, without masks or sensors—using just a router.
Wearables versus Wi-Fi: supplement or substitute?
The goal isn’t to choose “smartwatch or router,” but to use complementary use cases:
- Wearables provide personal context, additional metrics (HRV, SpO₂, temperature), outdoor detection, and continuous contact.
- Pulse-Fi offers maximum convenience, frictionless use, and minimal cost inside homes or clinics, with environmental coverage and no batteries to charge.
In a connected home, both approaches might work together: Wi-Fi alerts about anomalies; wearables confirm and detail. And if no wearable is used, the router at least monitors the essentials.
What does “clinical accuracy” mean?
The UC Santa Cruz publication describes “clinical-level accuracy”. Practically, it means that error margins relative to a reference device (oximeter) fall within clinically accepted ranges for tasks like resting pulse monitoring or tachycardia detection. Longer observation windows (e.g., 30–60 seconds) further reduce uncertainty. To turn Pulse-Fi into a medical device, it would require certification following regulatory standards (e.g., ISO 80601-2-61 for pulse oximetry, or FDA/CE guidelines for software as a medical device), which is a separate pathway from academic validation.
A practical step toward democratizing digital health
Since no wearables are needed, no cables required, and it does not depend on expensive sensors, Pulse-Fi aligns with the broader goal of digital health: enabling more people to benefit from remote monitoring. A router capable of listening to the heartbeat with error below 1 bpm in 5 seconds won’t replace a cardiologist but could send an early amber warning to prevent worse outcomes—at a cost of just a few dollars.
The authors welcome collaborations to bring this technology to market. If successful, a future where heart rate and respiration are “read in the air” at home will depend not on extra gadgets, but on activating a Wi-Fi feature already in place.
FAQs
What hardware does Pulse-Fi need?
It works with low-cost Wi-Fi transmitters and receivers. In the study, they used ESP32 boards (about $5–$10) and Raspberry Pi (~$30). Using higher-quality consumer routers could further improve accuracy.
How far and in what scenarios does it work well?
The system performed reliably with a person up to 10 feet away and in 17 contexts: sitting, standing, lying, walking, with device placement varied in the room.
What is the accuracy and how long does it take?
After processing just 5 seconds of data, the average error was 0.5 bpm. Longer windows improve precision.
What about privacy and regulation?
Pulse-Fi does not record images or sounds; it only analyzes Wi-Fi channel variations. Nonetheless, any real deployment should include local processing, User control, encryption, and informed consent. For medical use, formal certification following medical standards would be required.
Main source: University of California, Santa Cruz — “WiFi signals can measure heart rate—no wearables needed”, press release about Pulse-Fi and its publication at DCOSS-IoT 2025.
via: news.ucsc.edu. Photos by Erika Cardema/UC Santa Cruz